Living with OCD: Why your Brain Feels Like a Hamster Wheel
(And What Actually Helps).
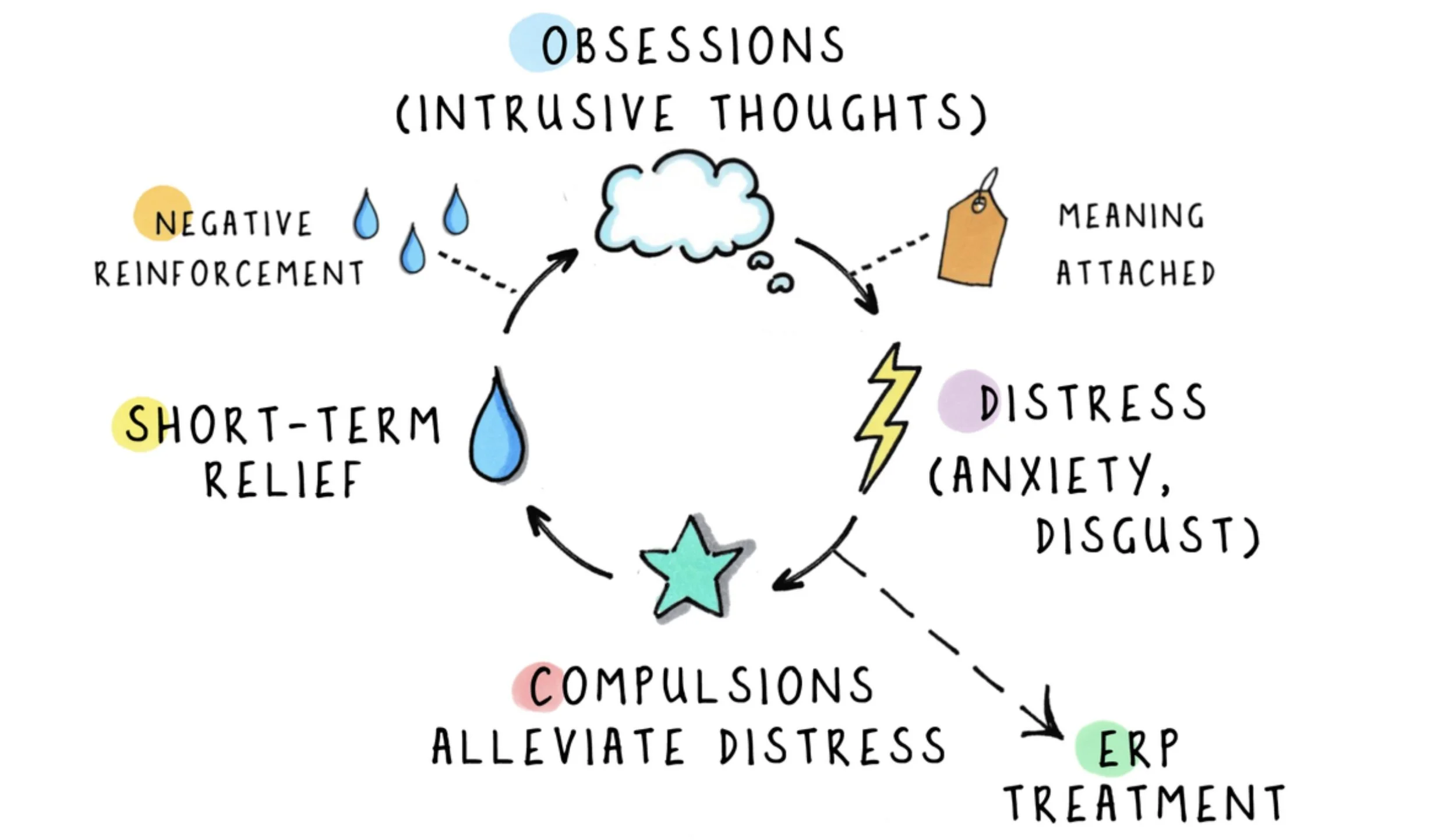
Let’s explore that relentless loop many people living with OCD know all too well. Imagine a hamster running in a wheel, over and over, thinking it’s getting somewhere, but never actually leaving the cage. That intrusive thought like “Did I leave the stove on?” or “What if something terrible happened?” pops up and triggers anxiety. Then comes the strong urge to do something, whether it’s checking, counting, repeating words, or some other behaviour that promises relief. It’s like the hamster trying to get a treat by running faster. But here’s the twist… every time the hamster runs faster, it actually strengthens the wheel and keeps it spinning. In other words, compulsions may feel helpful and provide temporary relief, but they make the loop tighter and longer. Each time a person living with OCD performs a compulsion, their brain learns, “This behaviour helps!” and the brain says, “Let’s do that again!” That is why compulsions make OCD stickier instead of lighter (Harvard Medical School, 2026).
from https://www.ocddoodles.com
*ERP Treatment = Exposure Response Prevention Treatment
So what actually helps slow down that hamster wheel? The best‑studied and most effective approach is Cognitive Behavioural Therapy with Exposure and Response Prevention. In plain terms, counselling lets a person intentionally face their triggers and refrain from the safety behaviour. Over time, the brain learns, “Wait, nothing bad actually happens when I don’t do that.” Think of it like teaching the hamster to step off the wheel and explore the cage safely instead of running endlessly. This retrains the nervous system to tolerate uncertainty and discomfort, which is the real engine behind OCD (Mayo Clinic, 2026).
There’s an exciting adaptation of traditional CBT called Inference‑based Cognitive Behavioural Therapy (I‑CBT). In a Divergent Conversations podcast episode, Dr. Megan Anna Neff and Patrick Casale spoke with Brittany Goff, a clinical social worker and I‑CBT pioneer, about how this approach helps people living with OCD, including those with diverse neurocognitive styles. I‑CBT focuses on the stories we tell ourselves about uncertainty and doubt, helping people gently question whether these inferences reflect reality. Brittany shared that using I‑CBT interrupts narratives of doubt in a powerful and immediate way (Divergent Conversations episode 141, 2026).
Mindfulness and acceptance‑based practices can also be helpful companions to these therapies. These strategies teach a person living with OCD to notice thoughts, feelings, and urges without reacting with compulsions. Think of it as watching clouds drift across a bright sky — the clouds are there, but they don’t control the sun. Early evidence shows that this approach may reduce distress around obsessions and improve quality of life when paired with CBT or I‑CBT (Hertenstein et al., 2025).
ADHD and autism are common co‑occurring conditions with OCD. ADHD’s distractibility and impulsivity can make compulsive loops feel even more urgent, because the urge to do something meets obsessive doubt face‑on. Autism can add sensory sensitivities, intense focus on detail, or routines that colour how OCD looks from day to day. This is one reason why counselling that is informed by neurodiversity matters. It honours each person’s unique wiring and supports them in ways that fit their lived experience (OCD‑UK, 2025; Rodgers et al., 2025) (divergentpod.com).
Here is the bottom line if this feels familiar: compulsions make the OCD loop tighter, CBT with ERP can be effective, I‑CBT offers another way to address how we interpret uncertainty, mindfulness helps with distress, and therapists trained in neurodiversity‑informed counselling can make all the difference. Doing therapy with a trained and certified mental health professional matters! These approaches are nuanced and most powerful when guided with compassion and understanding.
Now… imagine your hamster finally stepping off the wheel, sniffing the sunflower seeds on the floor, and pausing to stretch. It might wobble a bit at first, but eventually, it discovers there’s a whole world beyond the spinning wheel. That’s exactly what learning these therapies can feel like: a small, steady step off the wheel can open the door to a much bigger, calmer space in your mind.
Interested in Therapy?
If any part of this resonated with you and you’re curious about therapy, you don’t have to navigate this alone. See if we are a good fit by booking a free 15-minute consultation.
References
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.; DSM-5-TR). https://doi.org/10.1176/appi.books.9780890425787
Goff, B. (2023). Inference-based cognitive behavioral therapy for obsessive-compulsive disorder. Routledge.
Harvard Medical School. (2026). Obsessive-compulsive disorder (OCD): Symptoms and treatment. Harvard Health Publishing. https://www.health.harvard.edu
Hertenstein, E., Nissen, C., & Feige, B. (2025). Mindfulness-based interventions for obsessive-compulsive symptoms: A systematic review and meta-analysis. Clinical Psychology Review, 104, 102320. https://doi.org/10.1016/j.cpr.2024.102320
International OCD Foundation. (2026). Evidence-based treatments for OCD. https://iocdf.org
Mayo Clinic Staff. (2026). Obsessive-compulsive disorder (OCD). Mayo Clinic. https://www.mayoclinic.org
Neff, M. A., & Casale, P. (Hosts). (2026). OCD, I-CBT, and neurodivergent experiences (Episode 141) [Audio podcast episode]. In Divergent Conversations. https://www.divergentpod.com
OCD-UK. (2025). OCD and neurodiversity. https://www.ocduk.org
Rodgers, J., Krebs, G., & McConachie, H. (2025). Adapting cognitive behavioural therapies for autistic individuals with obsessive-compulsive disorder. Journal of Autism and Developmental Disorders, 55(2), 421–435. https://doi.org/10.1007/s10803-024-06012-7